Scientific report
„Pediatric Brain Monitoring with Information Technology (KidsBrainIT). Using IT Innovations to Improve Childhood Traumatic Brain Injury Intensive Care Management, Outcome, and Patient Safety”
Project code: COFUND-NEURON III ERANET – KidBrainIT
Reporting May 2019
This scientific report presents the final results of the Romanian team of the multi-center grant „Pediatric Brain Monitoring Using Information Technology (KidsBrainIT).” Using IT innovations to improve brain traumatic injuries among the child, management, outcome and patient safety ” the acronym KidsBrainIT.
After the latest statistical data available, every year, over 60,000 new cases of traumatic brain injury (TBI) are recorded in Romania, and the number is growing. Road accidents continue to be the main cause of cranial traumas, which often cause cognitive, affective and behavioral disorders, with a particular impact on families and society. Of these, an increasing percentage is represented by severe cranio-cerebral trauma in children.
Traumatic brain injury often generates cognitive problems, which are manifested by impairment of patient’s thinking and memory, cognitive disorders (attention, memory, language, perception), affective and behavioral are the most common and important. These deficits also have a major impact on families and society as it causes social dependence on patients, even in the absence of physical disabilities, affecting work capacity, family relationships, daily activities, and neuropsychological recovery is essential.
World Health Organization estimated that up to 90% of head injuries that receive treatment are mild, of which moderate and severe injuries represent 10%. In the European Union the yearly aggregate incidence of TBI hospitalizations and fatalities is estimated at 235 per 100,000.
Fortunately, TBI in children is much lower, without being able to make a reliable estimate because of research differences, but partial studies have shown that TBI in children represents about 14% of the total TBI. Also children have a higher incidence of increased intracranial pressure (ICP) following TBI than adults (80% vs. 50%) and it is a major cause of morbidity and mortality in the pediatric age group.
Currently, the immediate treatment of TBI in children is based on an accepted and established protocol for providing the first care measures and then for diagnosis and treatment in brain traumas based on vital functions, shock treatment, neurological diagnosis, imaging, immediate medical therapy and then establishing the need for surgery.
In the intensive care management of traumatic brain injury (TBI) patients, the routinely collected multi-parameter bedside physiological monitoring data that is available for clinical interpretation is under-used. Multicentre data collection and analysis of such ‘bigdata’ have been shown to generate new hypotheses and novel data analysis methods. Because of the age-related developmental differences in post-TBI physiological responses and outcome, a similar informatics based initiative in paediatrics is much needed to make huge advances in this field. Using innovative analytics on the high-quality paediatric TBI ‘big-data’ in our feasibility study, we showed that current cerebral perfusion pressure (CPP) management and raised intracranial pressure (ICP) treatment is sub-optimal. To improve outcome, we need to have both cerebral autoregulaton derived optimal CPP target thresholds and use an ICP dose-response approach that takes into consideration both the duration and magnitude of raised ICP.
As it is known continuous monitoring of intracranial pressure in real time is a standard in intensive care for severe cranio-cerebral trauma together with continuous blood pressure monitoring (MAP) allows the calculation of cerebral perfusion pressure (CPP) and the establishment of an optimal cerebral arterial infusion to improve treatments for severe cranio-cerebral trauma in children. Children aged between 2 and 16 years with cranio-cerebral trauma who require hospitalization and treatment in intensive care services are included in this study in three neurosurgical hospitals: Prof. Dr. N. Oblu Clinical Emergency Hospital Iasi , Emergency Clinical Hospital „St. Maria” Iasi and Emergency Clinical Hospital „Bagdasar-Arseni” Bucharest. In severe traumatic brain injury (TBI) in children maintaining an optimal cerebral perfusion pressure is essential for normal cerebral function, and this involves intact cerebro-vascular autoregulation to provide a stable blood perfusion for mean arterial pressure (MAP) variations.
Objectives of the research project
The aim of this study is to set up a new multi-centre, multi-disciplinary, multi-national intensive care informatics group for paediatric TBI (KidsBrainIT) for current and future hypotheses testing. We then aim to use the KidsBrainIT data-set in this proposal to test two clinically relevant hypotheses: After sustaining traumatic brain injury (TBI), paediatric patients with a longer period of measured cerebral perfusion pressure (CPP) maintained within the calculated optimal CPP (CPPopt) window have:
(1) an improved global clinical outcome, and
(2) better tolerance against raised intracranial pressure (ICP).
To achieve this aim, the team of the research project developed a multi-centre, multi-disciplinary, and multinational Paediatric Brain Monitoring and Information Technology Group (KidsBrainIT), which included a central data repository to store prospectively collected minute-resolution physiological, clinical, and outcome data. This infrastructure allowed analyses on sub-sets of the data to apply novel data models and calculated validated indices as metrics of clinical management quality that were fed back to clinicians working within units contributing to KidsBrainIT. Developing this type of infrastructure was essential for investigations on how feedback of clinical management quality indices influenced and improved future treatment in later phases of KidsBrainIT. Data from the KidsBrainIT central data-bank were used to test our hypotheses.
Methods and results
Within the team in Romania three neurosurgical hospital: „Prof. Dr. N. Oblu” Clinical Emergency Hospital Iasi, „Sf. Maria” Children Clinical Emergency Hospital Iasi and „Bagdasar-Arseni” Clinical Emergency Hospital Bucharest participated in this study that included children aged 2 to 16 years who require intensive care management after sustaining traumatic severe brain injury.
The contributing units have similar treatment protocols, which include:
‐ defined raised ICP treatment guidelines using osmo-diuretics as a first line medical treatment;
‐ using intravenous infusions of vasopressive drugs (noradrenaline infusion being the first choice) to drive mean arterial blood pressure to achieve a target CPP;
‐ sedation and muscle relaxant protocol;
‐ mechanical ventilation to control PaCO2 to low normal values;
‐ actively controlling core body temperature to normothermia.
Data collection:
Patients’ anonymised clinical data are collected; it includes the cause and nature of injury, age, Glasgow Coma Score (GCS) on admission and after acute non-surgical resuscitation, pupillary responses, initial radiological and computerized tomography (CT), operative and other treatment details. Each patient’s anonymised clinical data is linked to their physiological and outcome data in the KidsBrainIT data-bank using an anonymous study ID. Routinely measured physiological data in minute-resolutions are captured from the bedside monitors prospectively. All physiological data are anonymised prior to exporting, and then stored in the KidsBrainIT central data-bank. Outcome assessments are performed by each local team.
Data Analyses
CPPopt calculation and ICP doseresponse visualisation analyses are performed to test our hypotheses and determine if TBI patients with favourable outcome have longer periods of measured CPP within the calculated CPPopt ranges and an enhanced tolerance of raised ICP.
The accordance between CPPopt and actual CPP is calculated to evaluate the association with survival (GOS > 1) and favorable outcome (GOS >3):
‐ the percentage of time for which the actual CPP is within the recommended CPPopt range;
‐ the average difference between actual CPP and CPPopt;
‐ the average absolute difference between actual CPP and CPPopt;
‐ the average absolute difference when actual CPP is outside CPPopt range;
‐ the average difference where actual CPP is below CPPopt;
‐ the average difference where actual CPP is above CPPopt; and
‐ the previous criteria are used in a multivariate logistic regression model.
A total of 941 children with traumatic brain injury received medical care during this time in these three neurosurgical departments, including minor, medium and severe brain traumas. Thirty one patients needed intensive care and 9 children have been ICP and blood pressure monitored, but only four patients were included in this scientific project. As presented in the previous report in two cases the values of ICP were high and very high and cerebral decompression was performed; unfortunately, the initial clinical condition was extremely severe and evolution was not favorable in these cases. The third and forth patients monitored showed elevated ICP values up to 28-30 mm Hg and 30 – 40 mm Hg , which were medically treated.
During this time in our three neurosurgical departments there were a total of 941 children with traumatic brain injury and 31 patients needed intensive care and 9 children have been ICP and blood pressure monitored, but only four patients were included in this scientific project. The scientific report that on the mid-term results of this multi-center grant presented the three cases: two children with high and very high values of ICP and cerebral decompression, but not favorable evolution and the case of the third patient monitored with elevated ICP values up to 28-30 mm Hg, medically treated with a favorable evolution. The four case had oscillating high ICP values up to 30 – 45 mm Hg, but the extremely severe initial clinical condition has made its evolution not favorable.
 Figure 1 – Case of child with severe TBI and contiuous intracranial pressure monitoring
Figure 1 – Case of child with severe TBI and contiuous intracranial pressure monitoring
 Figure 2 The child with severe TBI and contiuous intracranial pressure monitoring
Figure 2 The child with severe TBI and contiuous intracranial pressure monitoring
 Figure 3 Medical devices used for contiuous intracranial pressure monitoring
Figure 3 Medical devices used for contiuous intracranial pressure monitoring
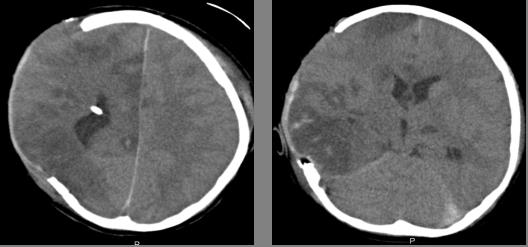 Figure 4 Child with with severe TBI and contiuous intracranial pressure monitoring with intraventricular catheter and cerebral decompression;
Figure 4 Child with with severe TBI and contiuous intracranial pressure monitoring with intraventricular catheter and cerebral decompression;
and CT of the same case with efficient decompressive craniectomy.
Discussion
Our number of 941 cases during this time should be interpreted by reference only for two areas in the country: two hospitals in Iasi and one in Bucharest, so it does not cover the entire our country. This number of cases of pediatric TBI vary across clinical and epidemiological studies and till now our number of cases with ICP and CPP monitoring are few and a statistical analysis could not be conclusive, but all the cases from the centers included in the grant from the other countries were hoping to have a statistical significance.
Intracranial pressure and cerebral perfusion pressure monitoring are invasive methods but they assured an early detection of increased ICP and disturbance of cerebral perfusion pressure in children with severe TBI. As we have mentioned in another material about this grant, the relationship between ICP elevation and CPP values is known in the adult, but in the pediatric TBI the studies are not conclusive; so “Chambers et al. proposed age stratified critical levels of CPP: in the age groups 2–6, 7–10, and 11–16 years, CPP values of 43 mmHg, 54 mmHg and 58 mmHg, respectively, were associated with normal values of ICP and good outcomes”.
Within the partnership between the centers involved in the finalization of this scientific research it has been achieved a distribution of the research work packages/tasks by partner: (1) Kids BrainIT infrastructure development; (2) multi-centre multi-national patient recruitment into the project; (3) data extraction, central data-bank development and implementation; (4) outcome assessment (6 and 12 months); (5) data artefact detection and cleaning; (6) physiological data analyse; (7) novel technology sub-study and (8) MRI outcome sub-study.
Anonymised clinical and physiological data from different centres are uploaded successfully into the data-bank using a secure http data upload service which ensures secured and encrypted transfer of fully anonymised data only. There are 48 patients recruited successfully into the study to-date in all contributing centres.
An important novel technology sub-study refers to the hybrid diffuse optical technology device, which is available for testing in Barcelona and patients are recruited into this sub-study since Barcelona open for recruitment in May 2018.
In our recruited patients with ICP and CPP monitoring the performed maneuvers were drug therapy, CSF drainage and decompressive craniectomy in accordance with modern therapeutic guidelines. Treatment used sedatives, analgesics; hyperosmolar therapy as intravenous mannitol and hypertonic saline to control intracranial hypertension; mild hyperventilation; barbiturates, temperature control and prophylactic anticonvulsants. The routine steroid treatment in children with severe TBI is not conclusive; it has to be individualized and rather it is not indicated because the potential harm from infectious complications. Decompressive craniectomy was performed for controlling intracranial hypertension and it was effective at ICP reduction.
Conclusion
- The severe traumatic brain injury in children requires a multidisciplinary approach in each phase of management.
- The prompt diagnosis during the initial evaluation and then the multimodal monitoring must be followed by the management of intracranial hypertension. Continuous ICP and mean arterial blood pressure (MAP) monitoring allow calculation of cerebral perfusion pressure (CPP) and to establish of an optimal CPP. All of this has its role to minimize the pathophysiological damage to the brain.
- The goal of this study was to establish the best care for severe TBI children and to ensure a transfer to a wider clinical audience.
Congresses
7th Congress of the European Academy of Pediatric Societies, EAPS 2018, Paris. October 30 – November 3, 2018, Poster – 512 Lo, T.Y.M .; Piper, I .; Kanthimathinathan, H .; Morris, K .; Levin, R.; Agbeko, R .; Davies, P .; Thorburn, K .; Parks, C .; Weitz, J .; Depreitere, B .; Meyfroidt, G .; Sahuquillo, J .; Poca, M .; Iencean, S.M. KidsBrainIT, which closes the big-data loop in pediatric brain trauma research – concept, co-ordination and challenges
44th Congress of the Romanian Society of Neurosurgery , Timisoara.September 5-8, 2018, Oral presentation Iencean St M, Tascu A, Apetrei CA, Gheorghita C, Iencean A St. Continuous Intracranial Pressure Monitoring in Severe Traumatic Brain Injury in Children
Journals
Lo, T.Y.M .; Piper, I .; Kanthimathinathan, H .; Morris, K .; Levin, R .; Agbeko, R .; Davies, P .; Thorburn, K .; Parks, C .; Weitz, J .; Depreitere, B .; Meyfroidt, G .; Sahuquillo, J .; Poca, M .; Iencean, S.M. KidsBrainIT, which closes the big-data loop in pediatric brain trauma research – concept, co-ordination and challenges, Pediatric Critical Care Medicine, 2018, vol. 19, 6S, p 207;
Apetrei, C. Gheorghita, A. Tascu, A.St. Iencean, Tsz-Yan Milly Lo, Ian Piper, St.M. Iencean. Pediatric Brain Monitoring with Information Technology (KidsBrainIT) – ERA-NET Neuron Grant, Romanian Neurosurgery, 2018, 32 (2): 183-186
Iencean St M, Tascu A, Apetrei CA, Gheorghita C, Iencean A St. Continuous intracranial pressure monitoring in severe traumatic brain injury in children, Romanian Neurosurgery, 2018, 32 (S.): 73-74
St M Iencean, A Tascu, CA Apetrei, C Gheorghita, Tsz-Yan Milly Lo, Ian Piper, A St Iencean. Intermediate results in contiguous intracranial pressure monitoring in severe traumatic brain injury in children – ERA-NET Neuron Grant, Romanian Neurosurgery, 2018, 32 (4): 518-523
Lo, T.Y.M , Piper I, et al. KidsBrainIT: A New Multi-centre, Multi-disciplinary, Multi-national Paediatric Brain Monitoring Collaboration. Acta Neurochir Suppl. 2018;126:39-45.
Depreitere B, Güiza F, Piper I. et al. Cerebral Perfusion Pressure Variability Between Patients and Between Centres. Acta Neurochir Suppl. 2018;126:3-6.
Lo, T.Y.M.; Sullivan, E. et al. Abstract PD-041: Improving patient care through research and appreciating clinical excellence (Impact – ACE) – an innovative pediatric critical care improvement research programme Pediatric Critical Care Medicine. 19(6S):42, 2018
Lo, T.Y.M.; Piper, I.; Black, G. et al. Abstract P- 511: When is the optimal time to wake a brain trauma patient in the paediatric intensive-care unit (PICU). Pediatric Critical Care Medicine. 19(6S):206, 2018.
St.M. Iencean , A. Tascu, C.A. Apetrei, C. Gheorghita, Tsz-Yan Milly Lo, Ian Piper , A.St. Iencean. Continuous intracranial pressure monitoring in severe traumatic brain injury in children Available on line May 2019: Romanian Neurosurgery (2019) XXXIII, (2) www.journals.lapub.co.uk/index.php/roneurosurgery
DOI: 10.33962/roneuro-2019-020
Reporting period: January 2018 – December 2018
The scientific report presents the results of the Romanian team for the year 2018 of the multi-center grant „Pediatric Brain Monitoring Using Information Technology (KidsBrainIT).” Using IT innovations to improve brain traumatic injuries among the child, management, outcome and patient safety ” the acronym KidsBrainIT.
Continuous monitoring of intracranial pressure in real time is a standard in intensive care for severe cranio-cerebral trauma, and treatments for reducing intracranial pressure are required when it is increased above 20 mmHg or more. In Romania, children aged between 2 and 16 years with cranio-cerebral trauma who require hospitalization and treatment in intensive care services are included in this study in three neurosurgical hospitals: Prof. Dr. N. Oblu Clinical Emergency Hospital Iasi , Emergency Clinical Hospital „St. Maria” Iasi and Emergency Clinical Hospital „Bagdasar-Arseni” Bucharest. Continuous monitoring of intracranial pressure and blood pressure monitoring (MAP) allows the calculation of cerebral perfusion pressure (CPP) and the establishment of an optimal cerebral arterial infusion to improve treatments for severe cranio-cerebral trauma in children. Maintaining an optimal cerebral perfusion pressure is essential for normal cerebral function, and this involves intact cerebro-vascular autoregulation to provide a stable blood perfusion for mean arterial pressure (MAP) variations.
Cerebro-vascular autoregulation is impaired and poor in severe cranio-cerebral trauma, and the degree of dysfunction varies over time in the same patient and in different patients, so optimal CPP is likely to vary with severe TCC management in children relative to lesion evolution and individually depending on your personal characteristics.
The activities carried out in stage II – 2018 included:
- Continue the documentation on the topic proposed by the study of the medical literature with the verification of the new data published in the specialized literature in 2018 and the dialogue and the exchange of opinions with the research teams from the other grant centers and observing the research protocol and checking the criteria selection of pediatric patients with severe post-traumatic cranio-cerebral trauma with the inclusion and exclusion criteria from the study.
- Analyze and track the evolution of pediatric patients admitted to cranio-cerebral trauma, identifying post-traumatic coma patients and assessing the diagnostic and therapeutic need for PIC monitoring in each case.
- Selection and recruitment of patients with severe cranio-cerebral traumas with post-traumatic coma and monitoring of intracranial pressure and transmission of data to the KidBrainIT database.
- Analysis of the results for patients studied and dissemination of these results, respectively their presentation at conferences, congresses and their publication in specialized journals.
Monitoring of pediatric patients hospitalized with serious cranio-cerebral trauma in a traumatic coma.
The children included in this study between the ages of 2 and 16 suffered a severe cranio-cerebral trauma with post-traumatic coma and were hospitalized in intensive care units in three neurosurgery hospitals: Emergency Clinical Hospital „Prof. Dr. N. Oblu „Iasi,” Emergency Hospital for Children „St. Iasi” and „Bagdasar-Arseni” Emergency Clinical Hospital Bucharest.
In these hospitals there are the same diagnostic and treatment protocols that are basically the same in the whole country: after the first emergency measures to diagnose and provide an effective primary assessment – ABC in an emergency, clinical and imaging diagnosis with the determination of the type of cranio-cerebral lesion is made. Depending on the diagnosis, the need for monitoring intracranial pressure in the case of intracranial hypertension syndrome and / or the opportunity for a neurosurgical surgical intervention is established.
The treatment schedule for intracranial hypertension syndrome comprises: surgery if necessary,
neurosurgical fitting of the intracranial pressure sensor and monitoring intracranial pressure and cerebral perfusion pressure, the application of increased intracranial pressure drop-down treatment using osmotic diuretics as a first-line medical treatment; sedation and muscle relaxation medication;
mechanical ventilation to keep PaCO2 at normal values; the use of intravenous vasopressor medications to maintain the mean blood pressure at values that provide normal cerebral perfusion pressure; actively controlling temperature while maintaining normothermia.
Anonymous patient clinical data were collected, corroborated with the cause and nature of lesions, age, Glasgow Coma score (GCS) upon arrival in the hospital and after resuscitation in the emergency receiving unit, if appropriate, pupil responses, radiological exploration and computer (CT) and / or MRI exploration, operator details and other treatments. As predicted in the scientific project, after the presidential monitoring was installed, the cerebral perfusion pressure was calculated by determining optimal CPP values. Next, individualized therapy is performed and the response to normalization of intracranial pressure and cerebral perfusion pressure is pursued. Clinical and imaging assessment determines whether patients monitored with favorable results have longer CPPs measured within the calculated CPPopt intervals and if they have increased tolerance for increased intracranial pressure. This determination allows completion of increased PIC therapy with the observation and correction of cerebral perfusion pressure in the calculated optimal CPP ratio.
In the three neurosurgery services involved in this project, there were a total of 624 children with cranio-cerebral trauma of different severity – from minor traumas with or without scalp wound to severe coma-like tarnations – of which one the number of 20 patients had severe cranio-cerebral trauma and required hospitalization in intensive care units, and 6 of them had presidential monitoring, but only 3 patients were included in this scientific project. In two cases ICP values were high and very high, and cerebral decompression was performed; unfortunately, the initial clinical condition was extremely severe and the development was not favorable in these two cases. The third patient monitored showed elevated ICP values up to 28-30 mm Hg, which were medically treated and the patient had a favorable progression.


The number of cases of children with cranio-cerebral, median and severe traumas varies according to clinical and epidemiological studies and the number of over 600 cases analyzed should be interpreted by reference to only two neurosurgical centers: two hospitals in Iasi and one in Bucharest , so only for two regions in the country. Cases of PIC and CPP monitoring are few due to inclusion criteria and a statistical analysis is not yet conclusive. For the cases requiring PIC monitoring, gender distribution is predominantly masculine, and the most common cause was the road accident.
Intracranial pressure monitoring is an invasive method, but has ensured an early detection of PIC growth in children with severe cranio-cerebral trauma. In the analyzed cases of traumatic intracranial hypertension monitored, the maneuvers performed were decompressive craniectomy, drug therapy and CSF drainage, according to modern therapeutic protocols.
The relationship between PIC elevation and CPP values is known in adult, serious crnio-cerebral traumatism analysis in children in the literature is not conclusive; so Chambers et al proposed critical CPP cerebral perfusion levels with age-related values: in the 2-6, 7-10 and 11-16 age groups, CPP values of 43 mmHg, 54 mmHg, and respectively, 58 mmHg were associated with normal intracranial pressure and good clinical outcomes. ”
The treatment used in the analyzed cases was performed according to national protocols consistent with those internationally accepted: application of sedatives and analgesics; hyperosmolar therapy such as intravenous mannitol and hypertonic saline solution for controlling intracranial hypertension; mild hyperventilation; barbiturates, temperature control and prophylactic anticonvulsants. Steroid routine treatment in children with severe cranio-cerebral trauma is not conclusive; it has to be individualized and is not indicated for the potential for infectious complications. Decompressive craniectomy was performed to control intracranial hypertension and was effective for reducing intracranial pressure.
The study will continue with patient inclusion and PIC and CPP monitoring to deliver meaningful and beneficial results that allow setting standards for severe brain trauma in children.
The best care for serious traumatic brain injuries in children requires a multidisciplinary approach at each management stage. Initial assessment with prompt diagnosis and multimodal monitoring should be followed by intracranial hypertension management (PIC and CPP) to reduce brain damage. Intracranial pressure monitoring provided early detection of intracranial hypertension ascites in children with severe TCC.
The results of the study are directly transferable to clinical practice as no special equipment is needed, other than the one currently used for the daily physiological monitoring of the traumatized infant hospitalized in intensive care services.
Analysis of results for studied patients and the presentation at conferences, congresses and their publication in specialized journals.
Congresses
7th Congress of the European Academy of Pediatric Societies, EAPS 2018, Paris. October 30 – November 3, 2018, Poster – 512 Lo, T.Y.M .; Piper, I .; Kanthimathinathan, H .; Morris, K .; Levin, R.; Agbeko, R .; Davies, P .; Thorburn, K .; Parks, C .; Weitz, J .; Depreitere, B .; Meyfroidt, G .; Sahuquillo, J .; Poca, M .; Iencean, S.M. KidsBrainIT, which closes the big-data loop in pediatric brain trauma research – concept, co-ordination and challenges
44th Congress of the Romanian Society of Neurosurgery RSN 2018, Timisoara.September 5-8, 2018, Oral presentation Iencean St M, Tascu A, Apetrei CA, Gheorghita C, Iencean A St. Continuous Intracranial Pressure Monitoring in Severe Traumatic Brain Injury in Children
Journals
Lo, T.Y.M .; Piper, I .; Kanthimathinathan, H .; Morris, K .; Levin, R .; Agbeko, R .; Davies, P .; Thorburn, K .; Parks, C .; Weitz, J .; Depreitere, B .; Meyfroidt, G .; Sahuquillo, J .; Poca, M .; Iencean, S.M. KidsBrainIT, which closes the big-data loop in pediatric brain trauma research – concept, co-ordination and challenges, Pediatric Critical Care Medicine, 2018, vol. 19, 6S, p 207; doi: 10.1097 / 01.pcc.0000537969.02938.72
THAT. Apetrei, C. Gheorghita, A. Tascu, A.St. Iencean, Tsz-Yan Milly Lo, Ian Piper, St.M. Iencean. Pediatric Brain Monitoring with Information Technology (KidsBrainIT) – ERA-NET Neuron Grant, Romanian Neurosurgery, 2018, 32 (2): 183-186
http://www.roneurosurgery.eu/atdoc/1ApetreiCA_Paediatric.pdf
Iencean St M, Tascu A, Apetrei CA, Gheorghita C, Iencean A St. Continuous intracranial pressure monitoring in severe traumatic brain injury in children, Romanian Neurosurgery, 2018, 32 (S.): 73-74
http://www.roneurosurgery.eu/atdoc/abstracts.pdf
St M Iencean, A Tascu, CA Apetrei, C Gheorghita, Tsz-Yan Milly Lo, Ian Piper, A St Iencean. Intermediate results in contiguous intracranial pressure monitoring in severe traumatic brain injury in children – ERA-NET Neuron Grant, Romanian Neurosurgery, 2018, 32 (4): 518-523